 Luteal Phase Defect: A Common Hormone Imbalance
Luteal Phase Defect: A Common Hormone Imbalance
Low progesterone is one of the most common hormone imbalances women face. Depending on your age, it can create different challenges.
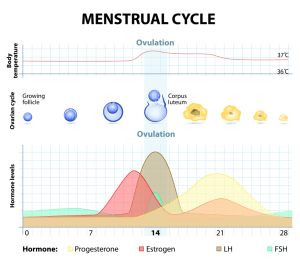
A middle-aged woman heading toward menopause might notice heavier, painful periods and mood changes. Periods might also be more frequent, because the second half of her cycle (the luteal phase) is getting shorter. This often happens when her ovaries produce too little progesterone after ovulation, or in some cases, fail to ovulate altogether.
The same thing can happen to a younger woman, and once again the challenge may be irregular or frequent periods. She could experience worsening PMS and mood changes. The younger woman may also find becoming pregnant more challenging. Implantation (when the fertilized egg attaches itself to the uterus) usually takes place 7-10 days after ovulation. If her period comes before implantation can occur, she is unlikely to conceive.
This brings us to the under-diagnosed problem we see in so many woman:
Luteal phase defect
After ovulation, the ovary should create enough progesterone to keep the uterine lining intact for an average of 12-14 days. This allows time for a fertilized egg to attempt implantation. If your luteal phase is 9 days or less, you have a luteal phase defect.
If you’ve had trouble getting pregnant, or you noticed your periods seem to come early, it’s possible that you have a luteal phase defect. It is worth noting that not every woman ovulates on day 14, so an “early period” might be normal for some. If you ovulate on day 10, for example, and your average luteal phase is 12 days, your period could come on day 22 of your cycle. If you were to do the math assuming a day 14 ovulation, you would incorrectly think you had an 8 day luteal phase.
So how do you know if you have a luteal phase defect?
Try collecting some data! This will help you and your physician to figure out the puzzle. Pick up a few packs of ovulation test strips (just like pregnancy tests, you get to pee on a stick). After your next period ends, begin testing every morning until you get a firm positive. In most cases, you will ovulate within 24 hours. You can then record that date and keep track how many days pass until your period arrives.
You will also want to get your hormones tests. Your doctor might ask for you to come in on day 3 or day 21 of your cycle depending on which hormones they are running. At the very least, you want to get a progesterone level on day 21 (if you ovulate around day 14). If you know that you ovulate several days before cycle day 14, or several days after, your doctor can adjust when they test for the hormone.
What causes a luteal phase defect?
Sometimes a short luteal phase is simply related to peri-menopause, and it might fluctuate month to month. In other cases, you want to speak with your doctor about the following possibilities:
-Over-exercise or malabsorption
-Thyroid disease
-Adrenal fatigue
-Ovarian cyst, Polycystic Ovary Syndrome
-High prolactin
-Metabolic disorder and insulin resistance
How do we treat a luteal phase defect with naturopathic medicine?
The key to regaining a normal luteal phase is understanding why it became short in the first place. This is the part where you and your physician get to be detectives. It might require a prescription, such as thyroid hormone if it turns out you have hypothyroidism. In other cases, diet and lifestyle changes may be enough.
Depending on what you and your medical team detect, effective naturopathic interventions often include:
-Diet changes and seed cycling
-Herbs such as Vitex and Black Cohosh
-Nutritional oils such as Evening Primrose, Flax or Borage
-Bio-identical progesterone therapy
-Stress reduction techniques
-Other specific nutrient therapies
Yours in health,
Dr. Kaley Bourgeois